Moyamoya
What is Moyamoya?
Moyamoya disease is a rare blood vessel (vascular) disorder in which the large arteries in the skull become blocked or narrowed, reducing blood flow to the brain. In an attempt to supply the brain with blood, tiny blood vessels then open up at the base of the brain.
The condition can cause a mini-stroke, stroke or bleeding on the brain. Moyamoya most commonly affects children but adults may have the condition.
“Moyamoya” is a Japanese term that means “puff of smoke,” which is used to describe the hazy appearance of these small vessels on an angiogram.
Call 314-362-3577 for Adult Patient Appointments or 314-454-2810 for Pediatric Patient Appointments
When arteries in the brain have been blocked or narrowed, individuals may experience signs of a TIA (transient ischemic attack) such as headaches, vision problems, the inability to think or speak clearly, numbness or weakness on one side of the body or seizures. Sometimes it is “silent” and there may be no symptoms at all.
Moyamoya is a result of the blood vessels creating new paths of delivery because of a blockage or narrowing of a larger vessel.
Individuals who have a higher risk for developing moyamoya would include those with sickle cell disease, neurofibromatosis, congenital heart disease, Down syndrome or if there is a history of cranial irradiation.
Moyamoya was first identified in people of Asian descent; however it is a world wide problem and crosses all ethnic groups. It is more common in females than males. Children are often diagnosed between the ages of 5-15. Adults are typically diagnosed in their 30’s and 40’s.
There may be a genetic link; research is currently investigating this possibility.
Cerebral angiography – an X-ray study of the blood vessels using a dye – is the principal form of imaging used for the diagnosis of moyamoya disease. The characteristic findings of moyamoya disease on an angiogram are traditionally described in stages, which progress from early narrowing of the carotid arteries to the formation of moyamoya vessels and then to the disappearance of these vessels with maintenance of blood flow by the external carotid and vertebral arterial systems.
| Stage I | Narrowing of carotid arteries |
| Stage II | Initial appearance of moyamoya vessels |
| Stage III | Intensification of moyamoya vessels |
| Stage IV | Minimization of moyamoya vessels |
| Stage V | Reduction of moyamoya vessels |
| Stage VI | Disappearance of moyamoya vessels |
Suzuki J. Moyamoya Disease. Tokyo, Japan: Springer-Verlag; 1986.
Noninvasive imaging techniques also may be used in the diagnosis of moyamoya disease. When magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) demonstrate blockage of carotid arteries and moyamoya vessels on both sides, a cerebral angiogram is not needed for a diagnosis.
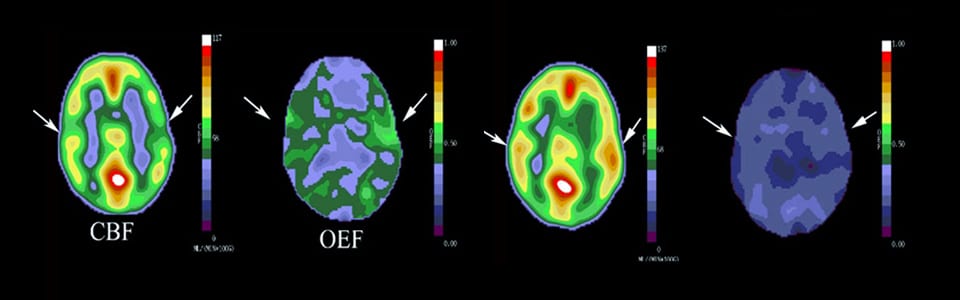
Once the diagnosis is confirmed, other imaging techniques may be used to measure blood flow and other aspects of the recovery and disease. Washington University neuroradiologists are experts in diagnosing and following moyamoya disease.
Treatment options and disease management are based on a collaboration between many specialties. Our treatment plans are tailored to the needs of each individual.
Medications – Some medications can reduce the risk of stroke and minimize further damage to the vessels.
Direct revascularazation– The superficial temporal artery is directly anastomosed (attached) to one of the intercranial arteries. This provides immediate improvement in blood supply to the brain and will continue to improve over time. This method is more frequently used for adults.
Indirect revascularazation– The superficial temporal artery or sometimes a portion of the temporalis muscle is laid directly on the surface of the brain to promote the new growth of arteries into the brain allowing for more blood flow. This is more frequently used for children.
Without treatment, this disease will progress, lead to further damage and put the individual at risk for stroke and/or death.
The loss of neurological function that occurs prior to intervention can be either permanent or short term.
Treatment can offer excellent long-term outcomes and have a significant impact on the reduction of future strokes.
What sets Washington University apart?
Leading national program
The Moyamoya Center at Washington University School of Medicine is a leading national program that is advancing the understanding and treatment of moyamoya disease.
Experienced multidisciplinary teams
Our neurosurgeons have performed surgical revascularization on hundreds of patients with moyamoya disease with excellent results. Patients with the disease are also treated by vascular neurologists who work closely with our neurosurgeons to provide the best care for each individual patient.
Patient stories

Caring for Kids: St. Louis Children’s Hospital
October 23, 2018
By: Julia M. Johnson, Town & Style
Many people know that a stroke can occur when a blood vessel in the brain ruptures or is blocked. But perhaps it’s less well-known that the condition doesn’t only affect adults. Washington University pediatric neurologist and critical care physician Dr. Kristin Guilliams of St. Louis Children’s Hospital says kids can experience a stroke at any age. “More than 4,000 pediatric strokes happen in the U.S. each year,” she says. “They actually are more common than brain tumors in children.” Read the full article. »