Cavernous Malformation
What is a cavernous malformation?
Call 314-362-3577 for Patient Appointments
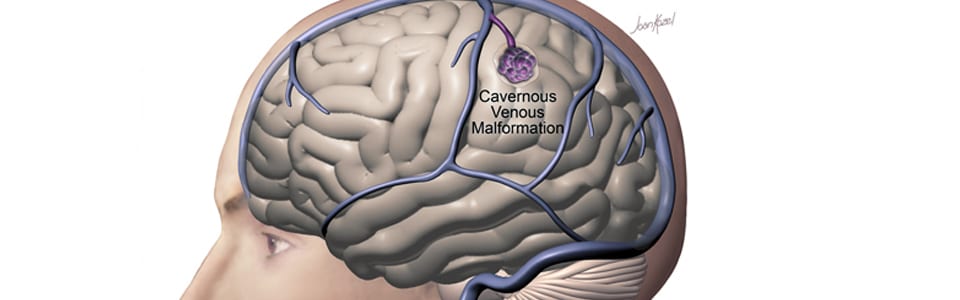
A cavernous malformation is an abnormal cluster of small blood vessels that resembles a raspberry or honeycomb. A person can have one or more cavernous malformations in their brain. Cavernous malformations occur in 0.5%-1% of the population and appear most often among people of Hispanic descent. Some cavernous malformations run in families, but most are sporadic (do not run in families).
Why rely on Washington University experts to treat your cavernous malformation?
Washington University cerebrovascular surgeons work as part of a multidisciplinary team to offer treatment for cavernous malformations at the Barnes-Jewish Hospital Stroke and Cerebrovascular Center, which is the only center in the region with an introperative MRi to assist with the removal of cavernous malformations.
The Center is among the most experienced in managing brain vascular malformations and receives physician referrals from across the country. In addition to cerebrovascular surgeons, other physician members of the treatment team include neurologists who specialize in interventional radiology as well as critical care and neuro-rehabilitation neurologists.
Treatment
Cavernous malformations are treated on a case-by-case basis. The treatment selected depends on the location of the cavernous malformation, the severity and nature of symptoms, the patient’s age and health status, and the risk involved in treatment. Treatment options include observation and surgery.
Observation
Often an appropriate choice for patients who are symptom-free, observation may also be appropriate for certain patients with symptomatic cavernous malformations who are older, have multiple medical problems or have a complex or difficult-to-reach cavernous malformation where treatment carries a high risk.
Surgery
Performed as an inpatient procedure, removal of the cavernous malformation from the brain is performed through open surgery. If successful, it provides immediate protection against brain bleeding and may also reduce or eliminate the risk of seizure. Surgery is a good option for many cavernous malformation patients; however, some patients have a complex or difficult-to-reach cavernous malformation that limits this treatment option.